You’ve probably heard of Ebola, and maybe even Marburg or Lassa fever, but what exactly do these viruses have in common? They’re all part of a terrifying family of diseases called viral hemorrhagic fevers, or VHFs for short. While their names alone might send a shiver down your spine, understanding them doesn’t have to. This article breaks down what makes VHFs so unique, how they spread, and what the chances are of encountering one in your lifetime.
VHFs are a group of illnesses caused by several distinct families of viruses. They can affect the body’s ability to control bleeding. Most patients experience only mild bleeding, like bruising or nosebleeds, though severe cases can lead to internal hemorrhaging or organ damage. While VHFs can cause fever, headaches, and muscle pain, some can lead to severe liver or kidney damage, while others cause shock or even death. The odds are low of catching these diseases.
Understanding Viral Hemorrhagic Fevers
Viral Hemorrhagic Fever (VHF) is a broad term encompassing a group of illnesses caused by several distinct families of viruses. These viruses share a common trait: they can compromise the body’s ability to regulate bleeding. Contrary to dramatic portrayals in movies, VHFs rarely cause patients to ‘bleed out.’ In reality, most individuals experience only mild bleeding symptoms, such as bruising or nosebleeds. However, severe cases can lead to internal hemorrhaging or organ damage.
These viruses aren’t particular about their targets. They can cause fever, headaches, and muscle pain, which sounds like your average flu — until things escalate. Some VHFs lead to severe liver or kidney damage, while others cause shock or even death. These viruses can cause fever, headaches, and muscle pain. While the odds are low of catching these diseases, understanding their nature is crucial for preparedness and prevention. Proper hygiene, awareness of potential exposure risks, and adherence to public health guidelines can significantly minimize the risk of infection.
Origins and Reservoirs of VHFs
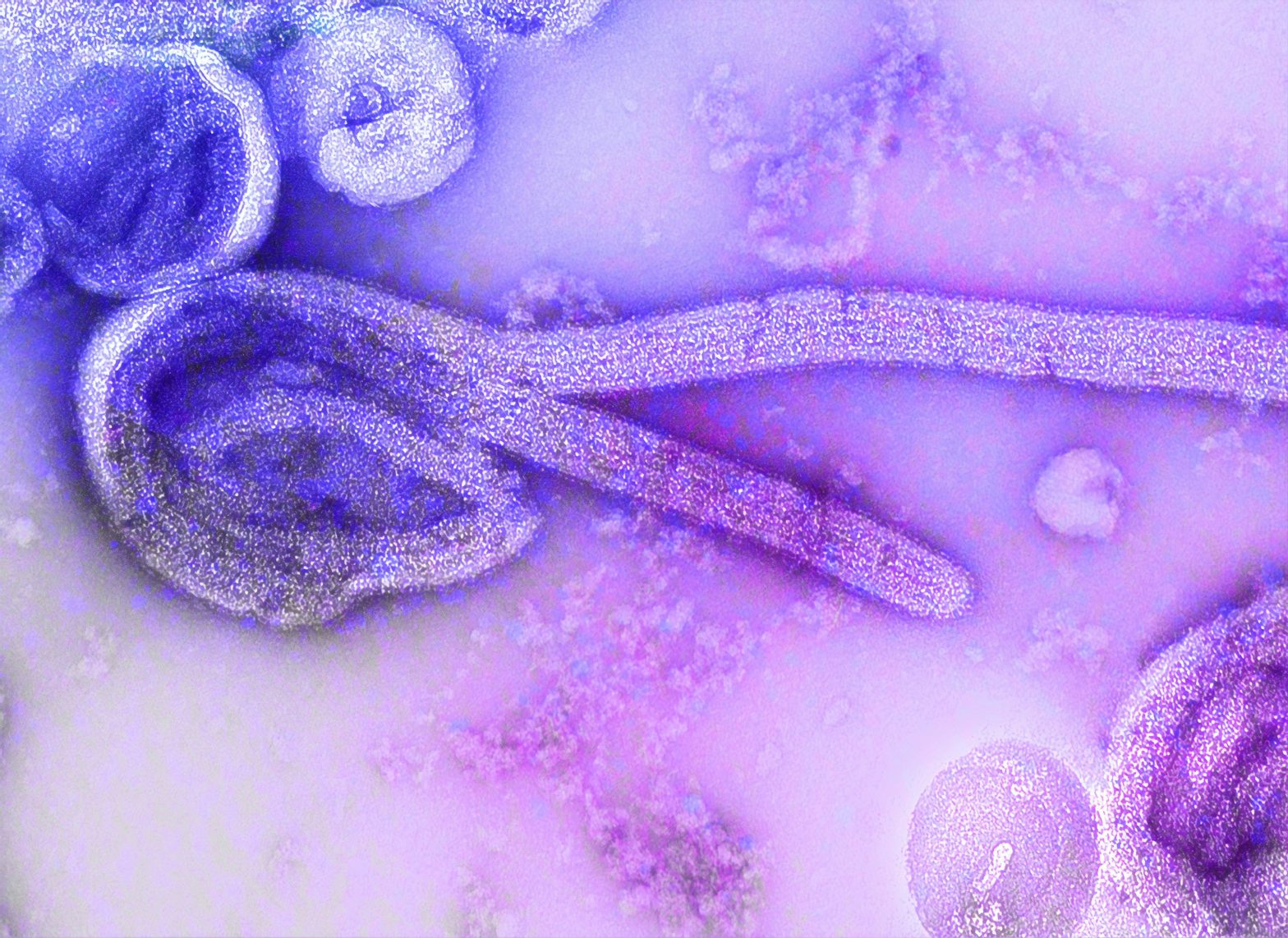
VHFs are zoonotic, meaning they jump from animals to humans. Rodents, bats, and insects like ticks or mosquitoes are often the carriers. Viruses might lurk in the saliva of a bat or the droppings of a rat, waiting to infect a human host. For example, arenaviruses like Lassa fever have a rodent reservoir. Mice can carry the virus without harm, but humans can be infected through urine-contaminated food or surfaces. Filoviruses, like Ebola and Marburg, likely jump to humans from bats.
These viruses are specific to their habitats. You won’t find Ebola in an Alaskan tundra or Lassa fever in Paris. They stick to regions where their animal hosts live, like parts of Africa, South America, or Asia. However, with global travel, infected patients can carry these diseases to regions where they aren’t naturally found. Understanding the zoonotic nature of VHFs is crucial for preventing outbreaks. Public health initiatives focused on monitoring animal populations, promoting safe food handling practices, and educating communities about potential exposure risks can help minimize the risk of spillover events.
Transmission Dynamics of VHFs
Some VHFs like dengue or yellow fever are spread by mosquito bites, while others require close contact. Transmission often occurs through bodily fluids: blood, saliva, or even sweat. This is why outbreaks often hit hardest in healthcare settings or close-knit communities. During the 2014–2016 Ebola outbreak, breaking the chain of transmission in overburdened healthcare systems was a major challenge. Simple measures like proper hand washing became life-saving interventions.
Controlling the spread of VHFs requires a multi-faceted approach that includes strengthening healthcare systems, promoting infection control practices, and educating communities about modes of transmission. Ensuring access to protective equipment, implementing robust surveillance systems, and fostering community engagement are essential components of effective outbreak response strategies. Additionally, investing in research to better understand the transmission dynamics of VHFs can inform the development of targeted interventions to prevent future outbreaks.
Assessing the Risk of VHF Exposure
If you’re reading this from North America or Europe, VHFs are rare. However, travelers to endemic regions or those working in fields like wildlife research or healthcare in outbreak zones should take precautions. Avoid contact with rodents, use mosquito repellents, and practice safe hygiene. Fortunately, some VHFs are preventable with vaccines. Yellow fever has a highly effective vaccine, and there are two licensed vaccines for Ebola (to be used only in places where the disease is present). Efforts are underway to develop similar protections for others.
Individual risk of exposure to VHFs depends on various factors, including geographic location, occupation, and lifestyle. Travelers to endemic regions should consult with healthcare professionals to assess their risk and receive appropriate vaccinations and preventative measures. Individuals working in high-risk occupations, such as healthcare workers or wildlife researchers, should adhere to strict safety protocols to minimize their risk of exposure. By staying informed and taking proactive steps to protect themselves, individuals can significantly reduce their risk of contracting VHFs.
The Future of VHF Research and Prevention
With climate change, urbanization, and global travel, VHFs have opportunities to spread like never before. Scientists are working to develop new treatments, vaccines, and rapid diagnostic tools. Advances in understanding these viruses’ genetic makeup could also lead to breakthroughs in stopping them in their tracks. Modern medicine, public health efforts, and common sense can make a world of difference in controlling outbreaks.
Continued investment in research and development is essential for advancing our understanding of VHFs and developing effective strategies for prevention and treatment. International collaboration and data sharing are crucial for monitoring emerging threats and coordinating global response efforts. By working together, scientists, healthcare professionals, and policymakers can strengthen our collective capacity to combat VHFs and protect global health security. Science and humanity have beaten big challenges before, and viral hemorrhagic fevers, as formidable as they seem, are no exception.
Final Thoughts and Actions
So, should you start stocking up on hazmat suits? Probably not. But it’s worth marveling at how these tiny pathogens wield such power over human health. You might want to donate to organizations working in places where VHFs are present, helping local populations stay safe. And you could work on reducing the impact of climate change, keeping mosquitoes where they are now, instead of expanding their range.
While VHFs may sound scary, the combination of modern medicine, public health efforts, and good old-fashioned common sense can make a world of difference in controlling outbreaks. For now, stay curious, stay informed, and maybe give a little extra respect to your neighborhood mosquito. (But not too much — they’re still jerks.)