When we think about cancer, our minds often jump to genetics, lifestyle choices, or environmental factors. We put on sunblock when we go out in the sun, avoid smoking, and install radon detectors in our homes. If we have a family history of cancer, we tend to worry about an ache or pain (or mass) we detect in an unusual part of our body.
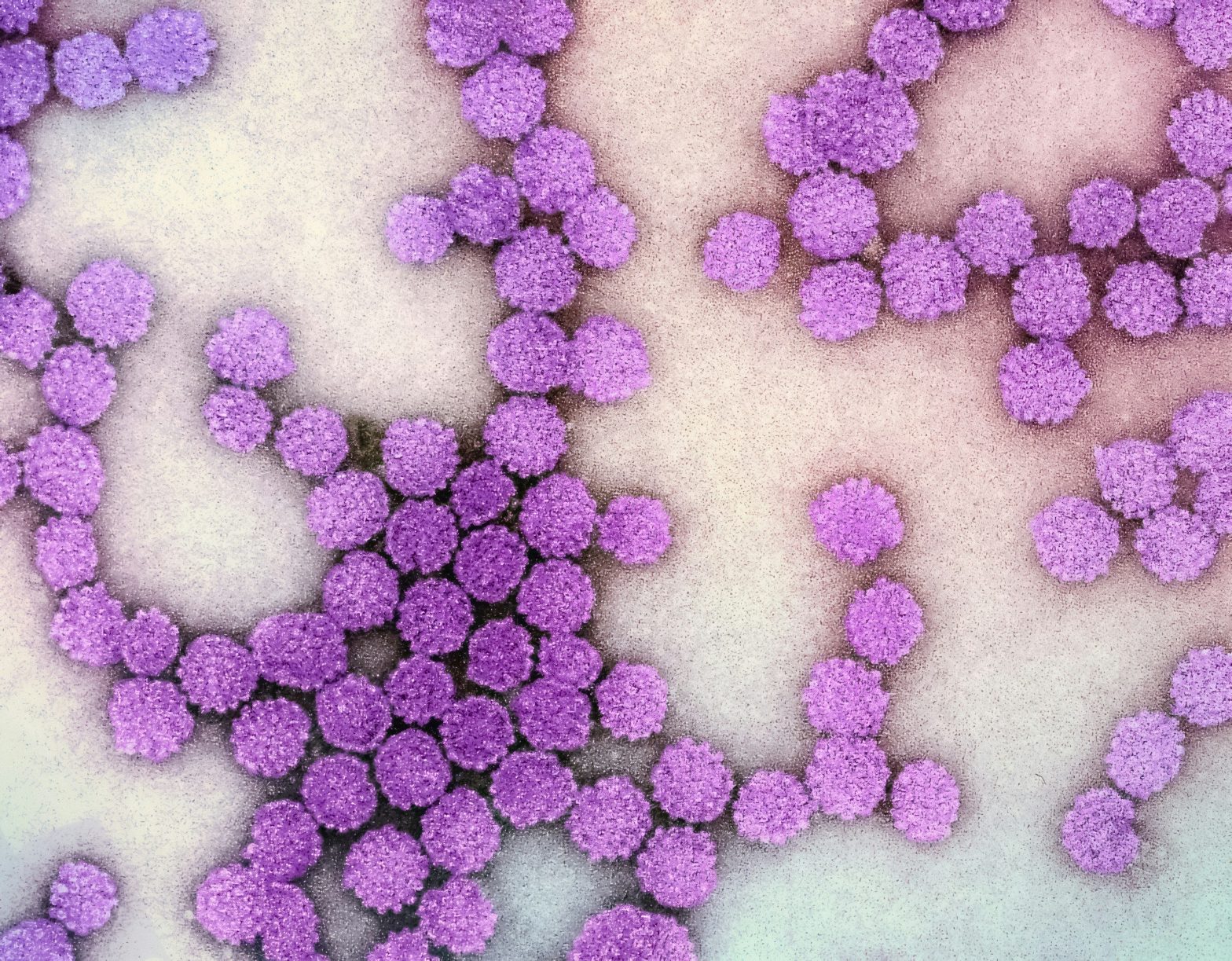
Don’t get me wrong. That’s all fine and good. But did you know that certain viruses can cause cancer? While not every infection leads to a malignancy, a handful of viruses have been scientifically linked to specific cancers. These viruses, known as “oncoviruses,” (onco- meaning “tumor” or “mass”) have sparked interest because of their unique mechanisms and potential for prevention through vaccines and other strategies.
As with any other virus, prevention is key. But let’s also talk about what you can do if you are exposed and infected. So let’s go one by one, and talk about these nasty little pieces of enveloped (or not) genetic material that hijack your cells and cause disease.
How Viruses Trigger Cancer: The Mechanisms at Play
First, let’s talk about how these oncoviruses actually cause cancer. It doesn’t happen overnight. Instead, they use a combination of mechanisms, leading to genetic mutations and chronic inflammation that disrupt normal cell function, including a cell’s ability to self-destroy when it needs to.
Some viruses, like human papillomavirus (HPV) and Epstein-Barr virus (EBV), produce viral proteins called oncoproteins. These proteins interfere with key cellular processes, such as cell cycle regulation and apoptosis (programmed cell death). For instance, HPV’s E6 and E7 proteins disable tumor suppressor genes like p53 and Rb, paving the way for uncontrolled cell growth. Similarly, EBV produces proteins like LMP1, which promotes cell survival and proliferation.
Chronic infection is another critical factor. The chronic inflammation caused by chronic infection leads to repeated cycles of cell injury and repair, increasing the likelihood of DNA mutations over time. Chronic inflammation also creates an environment rich in reactive oxygen molecules, which can directly damage DNA. (This is also known as oxidative stress.)
Other viruses hijack the host’s immune system. They evade immune detection and alter cytokine signaling, creating a microenvironment that supports cancerous growth. (Cytokines are chemicals used by cells to communicate, or to destroy foreign cells and microbes.)
Some oncoviruses incorporate their genetic material into the host genome. This integration can disrupt normal cellular functions and trigger mutations that lead to malignancy.
Finally, retroviruses can activate oncogenes through insertional mutagenesis. That’s a fancy way to say that by integrating their genome near a host oncogene, these viruses push the host cell into overdrive. That leads to the unregulated multiplication of those cells.
Let’s look at these viruses in more detail.
Human Papillomavirus (HPV) — A Preventable Threat
Human papillomavirus, or HPV, is perhaps the most well-known cancer-causing virus. Linked to cervical, anal, and oropharyngeal cancers, HPV spreads through sexual contact. The United States sees around 14 million new infections each year, with persistent “high-risk” strains like HPV-16 and HPV-18 being the culprits behind most HPV-related cancers. These strains have a notorious role in nearly all cases of cervical cancer, a substantial portion of anal cancers, and an increasing number of oropharyngeal cancers, particularly in men.
Symptoms can range from genital warts to precancerous lesions, but often, infections are without symptoms (asymptomatic), silently persisting until complications show up. The good news? Vaccines like Gardasil and Cervarix (the latter no longer used in the United States) effectively prevent infections from the most dangerous HPV strains. Vaccination campaigns have made strides in reducing cervical cancer incidence worldwide, as seen in Australia, which is on track to eliminate cervical cancer. (Elimination means the disease is extremely rare, not eradicated, which means it no longer happens at all.) However, the situation in the United States reveals persistent disparities that highlight the urgent need for equitable vaccination efforts.
Disparities in HPV Vaccination in the U.S.
Despite the availability of vaccines, vaccination rates are uneven across ethnic and socioeconomic groups in the United States. Studies reveal that Hispanic and Black populations, who face disproportionately higher rates of HPV-associated cervical cancer, are less likely to receive the HPV vaccine due to barriers such as limited healthcare access, cost, and cultural stigmas surrounding discussions of sexual health. These disparities are further exacerbated in rural areas, where access to preventive healthcare, including vaccines, is limited.
Notably, vaccination rates also vary by gender. Although HPV vaccines have been recommended for both boys and girls since 2011, girls continue to be vaccinated at higher rates than boys. This discrepancy may stem from the misconception that HPV-related cancers primarily affect women. However, HPV-related oropharyngeal cancers increasingly affect men, which now surpass cervical cancer in incidence in the U.S. Vaccinating boys is essential not only to protect them, but also to reduce transmission, achieving herd immunity. (Think of boys as the vectors in controlling HPV infection and disease.)
Closing the Gap
To address these disparities, public health initiatives must prioritize equal access to HPV vaccination for all ethnic and socioeconomic groups. Strategies include offering the vaccine free of charge through federal and state programs, integrating vaccination education into school curricula, and tailoring outreach efforts to address cultural concerns and misconceptions. Targeted efforts in underserved communities, such as mobile vaccination clinics and multilingual health education campaigns, can help overcome barriers to access.
Equally important is the normalization of vaccination for boys. Public health campaigns must emphasize that HPV vaccination protects against many cancers, including those that disproportionately affect men. By reframing the conversation to include all genders, we can challenge stigmas and ensure that boys and girls alike are vaccinated at equitable rates.
The push for universal HPV vaccination is not just about reducing individual cancer risks; it’s about achieving health equity and protecting future generations. By addressing these disparities and fostering equal access, the U.S. has the opportunity to replicate Australia’s success in drastically reducing HPV-related cancers and ultimately eliminating cervical cancer. Let’s hope we get there one day, along with the rest of the world.
Hepatitis B and C — Silent Causes of Liver Cancer
Both hepatitis B virus (HBV) and hepatitis C virus (HCV) are major contributors to liver cancer. These viruses cause chronic infections that can lead to cirrhosis and eventually hepatocellular carcinoma (cancer of the liver cells). HBV spreads through bodily fluids, while HCV is primarily bloodborne, both often linked to needle sharing or unsafe medical or sex practices.
Symptoms of liver damage might not appear until the disease is advanced, emphasizing the need for regular screenings. Vaccines are available for HBV, offering robust protection, but no such option exists for HCV yet. For those already infected, antiviral therapies can suppress the virus and reduce the risk of cancer development.
Epstein-Barr Virus (EBV) — The Versatile Oncovirus
Best known as the cause of mononucleosis, the Epstein-Barr virus is implicated in various cancers, including Burkitt’s lymphoma and nasopharyngeal carcinoma. It spreads through saliva, earning it the nickname “the kissing disease.”
Genetic susceptibility is one critical factor in EBV-related cancers. Specific genetic variations can make individuals more vulnerable to the oncogenic effects of EBV. For example, polymorphisms (differences in genes) in immune-regulation genes may impair the body’s ability to keep EBV latent or respond effectively to infected cells. Additionally, nasopharyngeal carcinoma, strongly associated with EBV, shows higher prevalence in certain ethnic groups, such as people of Southern Chinese or Southeast Asian descent. This suggests a genetic predisposition that interacts with the virus to increase cancer risk.
Environmental factors play an equally significant role. Chronic exposure to carcinogens, such as nitrosamines in preserved foods or tobacco smoke, can amplify EBV’s oncogenic potential. These substances damage cellular DNA, compounding the risk of mutations in the presence of EBV infection. Infections like malaria also appear to synergize with EBV, particularly in sub-Saharan Africa, where co-infection significantly increases the risk of Burkitt’s lymphoma. Malaria weakens the immune system’s ability to suppress EBV, creating an environment conducive to unchecked viral activity and malignancy.
Immunosuppression is another crucial factor. Individuals with HIV/AIDS or those undergoing immunosuppressive therapy after organ transplants are at significantly higher risk of developing EBV-associated malignancies. In these cases, the immune system’s inability to control EBV reactivation allows the virus to promote cancerous changes in cells.
The Burden of EBV in Developing Nations
While EBV infections are ubiquitous, their consequences disproportionately affect developing nations, where environmental and healthcare challenges exacerbate the risk of EBV-related diseases. In sub-Saharan Africa, where malaria is endemic, the co-infection with EBV has made Burkitt’s lymphoma one of the most common childhood cancers. Limited access to healthcare delays diagnosis and treatment, leading to higher mortality rates compared to wealthier nations. Similarly, nasopharyngeal carcinoma is prevalent in parts of Southeast Asia, where cultural and dietary habits, combined with genetic predispositions, contribute to its incidence.
The lack of an EBV vaccine further compounds the burden in these regions. Preventive measures are minimal, and public health systems often lack the resources to provide widespread screening or early detection for EBV-related cancers. The disparity is stark: while developed nations can leverage advanced diagnostic tools and targeted therapies to manage EBV malignancies, individuals in low-resource settings are more likely to suffer worse outcomes due to delayed diagnosis and inadequate treatment.
Other Notable Oncoviruses
Human herpesvirus-8 (HHV-8), also known as Kaposi’s sarcoma-associated herpesvirus. This virus is most prevalent in sub-Saharan Africa, where it contributes to high rates of Kaposi’s sarcoma, particularly in individuals living with HIV/AIDS. The overlap of HHV-8 prevalence with regions heavily impacted by HIV has created a dual epidemic. Globally, Kaposi’s sarcoma is responsible for tens of thousands of cases annually, with mortality rates particularly high in low-resource settings due to limited access to antiretroviral therapy and cancer treatments.
Merkel cell polyomavirus (MCPyV), in contrast, has a more widespread but lower prevalence globally. It is linked to Merkel cell carcinoma, a rare but aggressive form of skin cancer. This cancer predominantly affects older adults and immunocompromised people, and is more commonly seen in North America, Europe, and Australia. While cases number only in the thousands annually, the disease has a high fatality rate due to its aggressive nature and tendency to metastasize quickly. Advances in immunotherapies have improved outcomes for some, but treatment remains challenging, particularly in regions with limited healthcare access.
Human T-cell lymphotropic virus type 1 (HTLV-1), associated with adult T-cell leukemia/lymphoma (ATLL), is most common in specific endemic regions, including parts of Japan, the Caribbean, Central and South America, and sub-Saharan Africa. The virus is transmitted through breastfeeding, sexual contact, and blood transfusions. While HTLV-1 infection is lifelong, only a small proportion of infected individuals develop ATLL, typically decades after initial infection. Nevertheless, the disease imposes a significant burden in endemic areas, with poor survival rates due to the aggressive nature of ATLL and the limited availability of effective therapies in many affected regions. Worldwide, HTLV-1 infection is estimated to affect 5–10 million people, with ATLL contributing to thousands of cancer cases annually. This is only an estimate, however. The true number might be higher, but is unknown because of lack of global testing.
Prevention and Public Health Impact
While infection with an oncovirus significantly increases cancer risk, it’s important to note that cancer is a rare outcome. Factors such as genetic predisposition, immune status, and coexisting environmental exposures also play crucial roles in determining the progression from infection to malignancy.
Prevention is the cornerstone of reducing virus-related cancers. Vaccination, safe sex practices, clean needle use, and early screenings are all critical strategies. Public health campaigns, like those targeting HPV and hepatitis B, have made significant strides in lowering cancer incidences globally.
In the U.S., virus-associated cancers account for about 10% of all cancer cases. While this is lower than the global average, it underscores the importance of continuing research, improving vaccine access, and raising awareness. Globally, these viruses underscore the diverse pathways through which infections contribute to cancer, and highlight global health inequities.
Regions with high prevalence often coincide with areas of limited healthcare infrastructure, compounding the burden of these cancers. Addressing these challenges requires targeted public health interventions, improved diagnostic capabilities, and accessible treatments to mitigate the impact of these virally induced malignancies.
Additional Reading
- American Cancer Society. “Viruses That Can Lead to Cancer.”
- MD Anderson Cancer Center. “7 Viruses That Cause Cancer.”
- Australian Department of Health. “National Strategy for the Elimination of Cervical Cancer in Australia.”
- Clinical Microbiology Reviews. “Viruses and Human Cancers: A Long Road of Discovery.”
- Yale School of Medicine. “The Virus Behind the Cancer.”
Certain viruses, known as oncoviruses, significantly elevate the risk of specific cancers, including cervical, liver, and lymphoma. These viruses manipulate cellular processes, leading to genetic mutations and chronic inflammation that disrupt normal cell function.
Prevention is the cornerstone of reducing virus-related cancers. Effective strategies include vaccination against HPV and Hepatitis B, safe sex practices, and avoiding needle sharing. Public health initiatives must prioritize equal access to vaccines, address cultural stigmas, and ensure widespread screening.
While virus-associated cancers account for a smaller percentage of cases in the U.S. compared to the global average, they highlight the importance of ongoing research and equitable healthcare access. Addressing these challenges through targeted interventions and improved diagnostics is crucial to mitigate the impact of virally induced malignancies and achieve health equity worldwide.